Summary: Cost of Medical Billing Services
In general, a business can expect to pay percentage based charges that range from 3% to 9% of collection per claim for third party medical billing services. Monthly administrative fees range from $200 to $1000 per provider for small practices.
These prices will vary based on whether you use a cloud hosted Software as a Service (SaaS) provider or an on-site solution.
What is Outsourced Medical Billing?
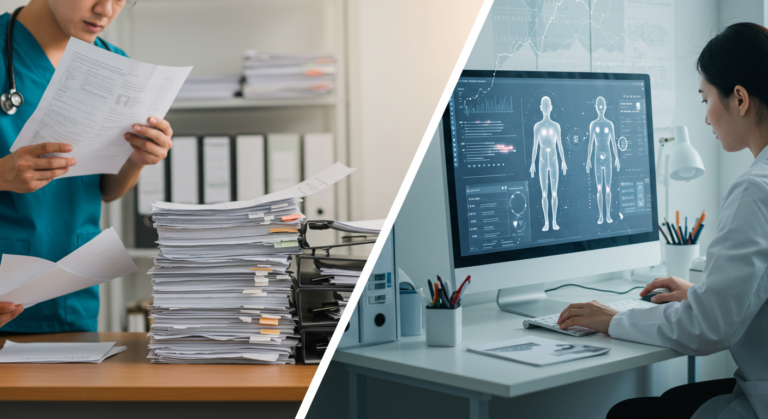
Running a business requires much more than expertise in the service that you are providing. For example, it takes one set of skills to be a medical practitioner, but running a successful medical practice is a different challenge entirely which requires different talent.
Outside of the medical practitioners themselves, the second most important aspect for any practice’s success is finance and billing. Without proper billing and payment management, medical practices will find it hard to be financially sustainable.
Because medical billing is a complex task requiring significant attention to detail, there are many third party vendors on the market who can provide billing expertise and management services. This frees up the leaders and managers of a medical practice to focus on what matters most to them—providing quality care.
Outsourced medical billing services are a great, affordable way to ensure that payments are conducted correctly with transparency to both the managers and the customers.
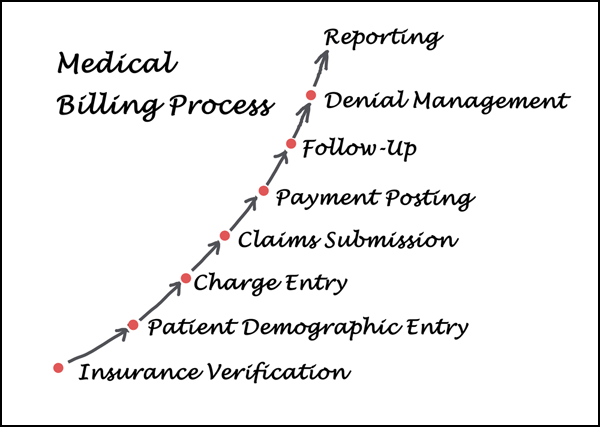
Curious about how medical bills are handled? Our guide to medical billing practices covers collection steps and industry regulations.
How Much Does a Medical Billing Company Charge?
For most medical billing services, there is a mix of up front, one time costs and monthly fees.
These up front costs can cover training, set up, administration, licensing, and more while the monthly fees can be for the software subscription, minimum monthly charges for use, or per collection charges that are done at a flat cost or percentage basis.
Medical billing companies typically charge fees based on:
- Percentage of collections fee: Ranges from 3% to 9% of the amount collected. This is a common model.
- Per claim fee: Some companies charge a flat rate per claim submitted/processed, such as $2-4 per claim.
- Monthly subscription: Fees for bundled services start around $200-300 per provider per month. Higher for additional services.
- Hourly rate: Some bill hourly for time spent processing claims, at rates from $30-60 per hour.
- Value-based pricing: A few bill based on value provided rather than simple volume. May involve benchmarks.
- One-time setup fees: Setup fees help cover onboarding costs and can range from a few hundred to over a thousand dollars.
- Minimum monthly fees: Even with percentage billing, some companies charge a minimum monthly fee to ensure a revenue baseline.
The pricing model that works best depends on your medical practice’s billing volume, revenue, and specific needs. Most established medical billing services charge within the range of 3-9% of collections or monthly subscription fees between $200-$1000 per provider.
Here are some general ranges of example prices that medical practices might pay for medical billing services:
Practice Size | Monthly Fee | Percentage of Collections |
Small Practice (1-3 Providers) | $200 – $1000 per provider | 5% – 9% of total revenue collected |
Medium Practice (4-10 Providers) | $800 – $3,000 per provider | 4% – 7% of total revenue collected |
Large Practice (11+ Providers) | $2,500 – $6,000+ per provider | 3% – 6% of total revenue collected |
Top Medical Billing Services Rates for 2024
Some common SaaS solutions and their rates are listed below. Because the costs of on-site solutions vary based on the specific needs of the client, contact the on-site provider for a tailored quote based on your organization’s requirements.
Medical Billing Service | Pricing |
4% to 8% collections rate or $1.42 per claim | |
Bundled billing and EHR services from $149 to $249 per month | |
7.9% to 10.9% with a one-time start-up fee of $1,297 and monthly minimum fee of $999 | |
Starts at $150 per provider | |
5% to 7% per claim with an option to do solely coding for $0.99 per claim | |
Monthly subscription fees starting at around $200 per provider | |
5-7% of collected revenue | |
Plans starting at $449/month for up to 50 claims | |
Plans starting at $179/month for basic services | |
Plans starting at $199/month | |
3-5% of collections | |
Around 5% of collections, plans from $350/month | |
Plans starting at $359/month |
Example Medical Billing Service Costs
Small Family Practice
- 1 doctor, ~1,500 patients
- $2,000 per month
- Full revenue cycle management
Cardiologist Practice
- 2 doctors, ~3,000 patients
- $3,500 per month
- Software, reporting, revenue cycle management
Mid-sized Orthopedic Clinic
- 4 doctors, ~10,000 patients
- $6,000 per month
- Dedicated account reps, insurance verification, resubmission
Large Multi-specialty Practice
- 10 doctors, 25,000 patients
- $12,000 per month
- Coding, claim scrubs, follow-up, denial management, analytics
Small Surgery Center
- ~300 procedures per month
- $1,500 per month
- Complete claim submission and reimbursement services
Other Cost Considerations
When shopping for a billing service provider, it is important to keep some things in mind.
1. Beware Excessively Low Costs
If a service provides a cost that is exceedingly lower than competitors, or is even a free to use platform, be aware that the quality of these services may not be up to the standards you require. These services may be performed by unqualified staff who are not as thorough as more robust and established providers.
Whoever you hire as your billing service, remember that you are entrusting them with your finances—a key component of your business that will make or break your organization.
2. Avoid Excessive Fees
While some fees such as administration, training, and set up are common, avoid businesses that have an excessive amount of other charges such as clearinghouse fees, patient statement fees, or customer support fees.
Always check with your prospective provider and ask for a quote on what the total cost would be while asking them to explain each and every charge.
3. Pay Attention to Monthly Minimums
While monthly minimum charges are common, be sure that your organization can afford to pay those rates regularly. This is especially important if you are a small firm or just starting out. Make sure your revenue is high enough to meet the minimum monthly fees while still being profitable.
Medical Billing Services FAQ
The average cost varies depending on practice size and service model, but typically ranges from 3% to 9% of collections for percentage-based pricing, or $200 to $1000 per provider for monthly subscription models.
The decision to outsource or keep billing in-house depends on various factors including practice size, budget, and expertise. Outsourcing can often lead to faster payments and improved cash flow, but in-house billing gives you more control. Consider your healthcare system’s specific needs and ROI when making this decision. Read our article on why hiring a medical billing service makes sense.
Fee-for-service is the traditional model where providers are paid for each service rendered. Pay-for-performance (or pay for performance) is a value-based model where providers are compensated based on the quality and efficiency of care provided, often leading to better patient outcomes.
Many medical billing services offer credentialing as part of their package. This involves verifying and enrolling healthcare providers with various insurance companies to ensure proper reimbursement.
Yes, some companies offer flat fees or flat fee structures for certain services. These might include a set price per claim processed or a fixed monthly rate regardless of the volume of claims.
Reputable medical billing services maintain trust through transparency, regular audits, and detailed reporting. They often provide stats on claim acceptance rates, time to payment, and other key performance indicators. Before signing a contract, ask about their quality assurance processes and error rates.
Medical billing services act as intermediaries between healthcare providers and insurance companies. They handle claim submissions, follow up on unpaid claims, manage denials, and negotiate with insurance companies on behalf of the healthcare provider.
Yes, professional medical billing services can often improve a practice’s financial performance by increasing clean claim rates, reducing denied claims, and accelerating the revenue cycle. This can lead to more consistent cash flow and potentially more money for the practice in the long run.
Medical Billing Conclusion
When utilized correctly, medical billing services can provide a huge boost to a medical practice’s efficiency and bottom line while freeing up medical professionals to focus on other aspects of patient care. These vendors provide comprehensive, professional, billing expertise that would otherwise be extremely expensive to produce internally. Compare medical billing service rates today with our free tool to get started!
Resources:




Leave a Reply